The Medical Treatment of Teenage Gender Dysphoria
07 juli 2023 | Forum for Democracy Intl
By Leontien Bakermans, PharmD and Dr Elisa Garcia, biomedical ethicist
A number of people feel a mismatch between their biological sex and how they feel. This is called gender dysphoria. In this article, we will discuss the medical treatment of 'gender reassignment' in young people and look at risks, side effects and whether there is an alternative treatment. We will finish with an ethical discussion.
DSM-5 and ICD-11
DSM-5 is the most recent version of the American Handbook of Mental Disorders. In this edition, 'gender identity disorders' has become "gender dysphoria, the psychological distress resulting from an incongruence between one's sex assigned at birth and one's gender identity" [i],[ii]. ICD-11, WHO's classification book for all disorders, both mental and medical, calls it 'gender incongruity' and has moved it to the category 'disorders related to sexual health', instead of keeping it in the chapter on 'mental and behavioral disorders', as this was considered too stigmatizing. [iii],[iv]
Sex is obviously not assigned at birth, but arises at fertilization, when the sperm and egg fuse, creating a new person who carries half of the father's and half of the mother's chromosomes. The sex chromosomes are either male or female and are present in every cell of the body. Changing this is impossible.
This means that, biologically, people cannot change gender. Biologically, therefore, a trans boy is not a boy and a trans girl is not a girl.
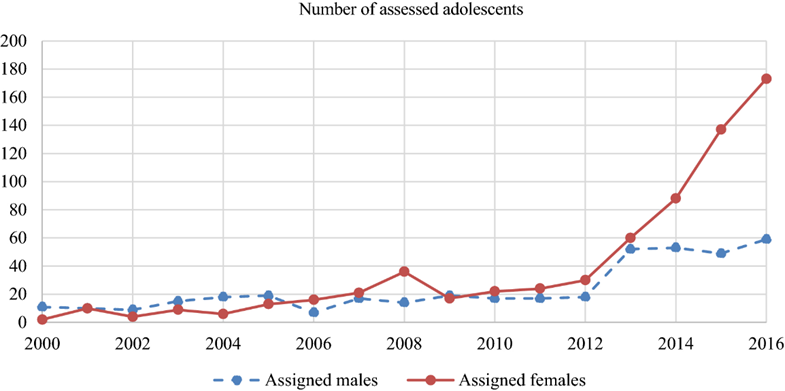
From 2012, there has been a sharp increase in the number of children referred to gender clinics with issues with their gender identity, girls now being represented three times as often as boys. Globally, it's the same picture. Data from the Knowledge and Care Centre for Gender Dysphoria at Amsterdam UMC (location VUmc) are shown in the chart[v] below.
In order to understand what gender treatment entails and which risks are involved, we first need to know which developments adolescents go through at puberty.
Puberty development
At puberty, the production of hormones begins. In the brain, substances called gonadorelin-releasing hormones (GnRH) are released, prompting the pituitary gland to make luteinising hormone (LH) and follicle-stimulating hormone (FSH). These hormones, in turn, signal the sex organs to make sex hormones: oestrogen in girls and testosterone in boys, see Figure 1.
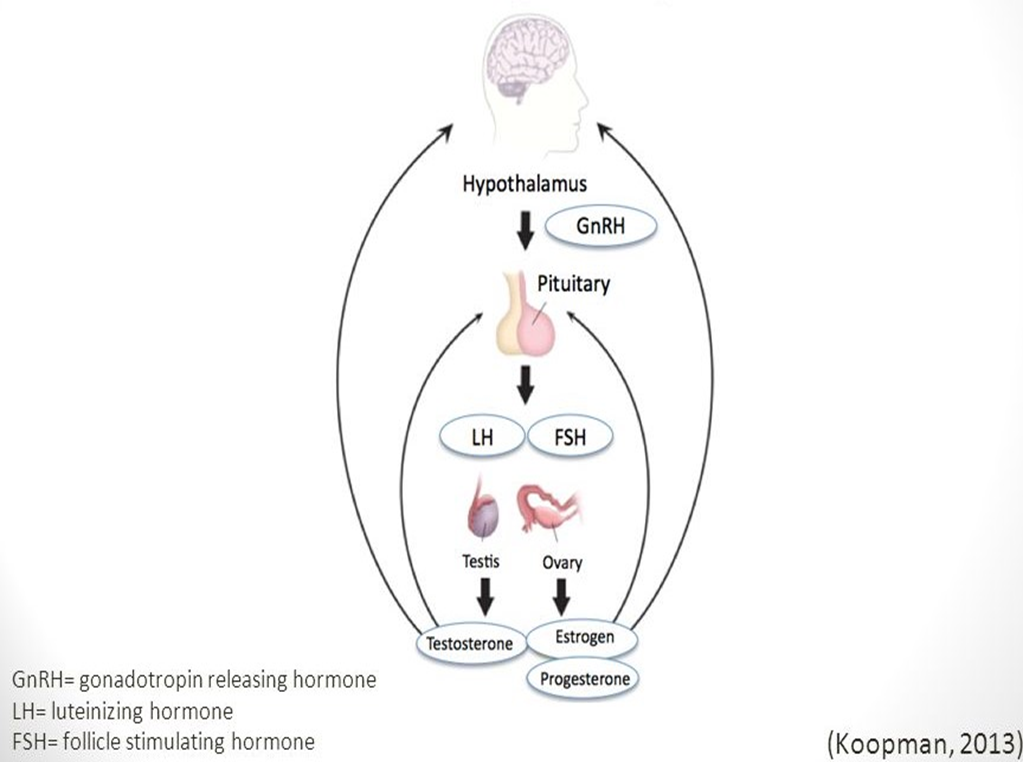
Figure 1
Oestrogen and testosterone are responsible for the development of secondary sexual characteristics:
- In girls, labia, vagina, uterus, and breasts develop and mature. Ovulation and menstruation begin to occur.
- In boys, the penis enlarges and erections and ejaculatory power develop. The voice becomes lower and facial hair appears.
This age phase is also important for brain and bone structure development. And a growth spurt takes place.[vi]
Brain and psychological development
Sex hormones are essential for brain development. Testosterone and oestrogen also influence emotions and feelings and this is reflected in behaviour. [vii] [viii]
In particular, the so-called prefrontal cortex in the brain undergoes a major development during adolescence. This cortex is important for the regulation functions of the brain and for things like decision making, planning, social behaviour and self-control.
Vulnerable
Children who want to change sex are a vulnerable group. They have above average mental health problems, such as autism, anxiety and depression.[ix] One in five transgender people has attempted suicide at least once, and more than two in three say they have had suicidal thoughts at some point. This is about 10 times as high as in the general Dutch population. [x]
The Dutch Protocol[xi]
For this group of children, the Knowledge and Care Centre for Gender Dysphoria at Amsterdam UMC developed the so-called Dutch Protocol, a treatment aimed at 'gender reassignment'. This protocol plays a pioneering role in the world.
First step: puberty blockers
The first step of the protocol is treatment with puberty blockers, which can be started from the first signs of puberty, at about 11 years of age. These heavy drugs were never registered for this indication. Officially, they are prescribed to chemically castrate sex offenders or to treat prostate cancer. There is also an indication for children who enter puberty too early (for example at the age of six), in order to delay their puberty until, say, age 12, to ensure that it is timely and parallel to that of peers.
These puberty blockers are so-called synthetic GnRH-like hormones, which shut down the action of natural GnRH. They also stop oestrogen or testosterone from being produced.
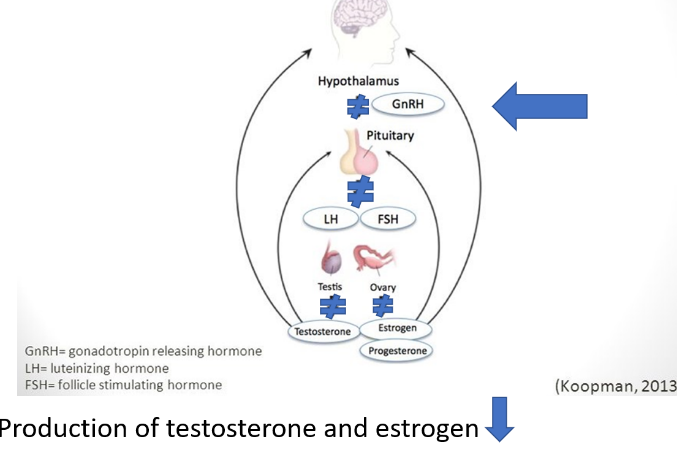
Figure 2
In this way, the progression of puberty is inhibited. This relieves the immediately distressing symptoms of gender dysphoria by preventing the outward sex characteristics from developing further. But it has other effects too.
Effect on fertility
In trans identified boys, sperm function stops. In order to enable them to still have children of their own, later in life, sperm may be frozen and stored. However, if no ejaculation has taken place yet and it is decided to do this in the course of the treatment, the puberty blockers should be stopped for at least three months to allow sperm cell production to start. And that is precisely something that trans-identified boys tend not to see. Also, there is no guarantee that a pregnancy will actually come about with the frozen sperm, if a potential (surrogate) mother is found at all.
In trans identified girls, ovarian function stops. They can freeze eggs for later. If they decide to do this during the course of treatment, they will have to stop the puberty blockers for three to six months.[xii]
The physical and mental impact/pain of ''harvesting'' eggs and sperm or testis tissue at such a young age is not to be underestimated. Also, it has not yet been scientifically studied.
Effect on bones
The higher the bone density, the stronger the bones. In the period before puberty, bone density increases by 5% per year, during puberty by 10% per year.
The use of puberty blockers stops this increase and prevents bone density from reaching its maximum. This increases the risk of weak bones and bone fractures later in life. [xiii] Figure 3 shows bone density without puberty blockers and after 1, 2 and 3 years of puberty blockers. The so-called z-score, measure of bone density, becomes negative.
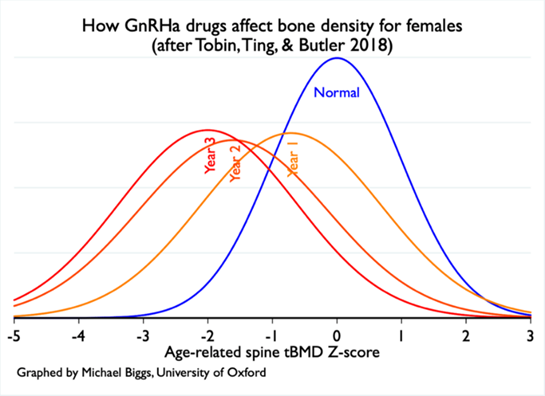
Figure 3
Effects on the brain and psychological effects
Suppressing sex hormones affects the development of the brain, in particular the prefrontal cortex. The effect of this change in development is still unclear. However, studies have shown that puberty blockers may cause poorer cognitive and executive functions (such as remembering, planning, reasoning, decision making and carrying out necessary actions) and a greater risk of depressive symptoms and other behavioural and emotional problems. [xiv]
Pause button?
The Amsterdam gender clinic says that "this period is meant to allow you to think calmly about whether you really want to take the step to transition to the opposite sex". The treatment is presented as pressing a simple 'pause button' that temporarily stops puberty. If desired, the treatment stops and puberty is supposed to resume. But is this really the case
In fact, it is not that common for children to stop taking puberty blockers.[xv] So, it is not used as a break, but as the first step of your transition, which you simply have to take. A step which turns out to be reversible only in theory. And the first step towards lifelong medicalization.
As a result, little research has been done to determine whether the stopping of puberty blockers is harmful and whether normal puberty is really resumed in these children. We know that hormonal levels often normalize only a year or more after stopping the blockers, thus prolonging puberty delay even more, resulting in an even longer inhibition of normal bone, brain and psychosocial development.
Meanwhile, these children alienate themselves from their peers, who do experience normal development and develop physically, intellectually and sexually, while the child on puberty blockers remains stagnant in all these areas. What this means for the child's social development is not named in any research.
Second step: cross-sex hormones
After the puberty blockers, most young people at the age of 15 or 16 continue with cross-sex hormones, i.e. the sex hormones of the desired sex.
Female-to-male patients are administered testosterone. This leads to the development of a low voice, a beard and body hair, a more masculine body shape, clitoral enlargement and further reduction of breast tissue.
In a male-to-female transition, administration of oestrogens results in breast development and a more feminine body shape.
Use of these hormones remains necessary for the rest of life, because the body does not make them itself. Some of the changes are irreversible though, such as a deeper voice, facial hair and baldness in trans men, and breast growth in trans women. [xvi]
Side effects
Side effects include a higher risk of heart attacks and strokes.[xvii]
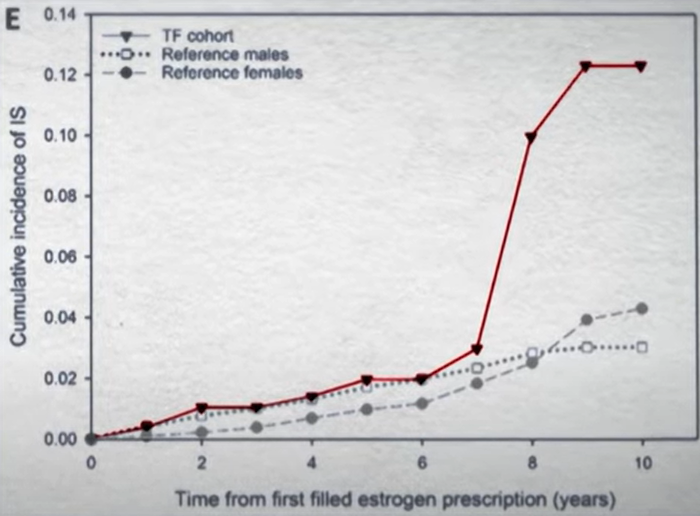
Graph from Swedish documentary Trans Train. Brain infarcts plotted against number of years of oestrogen use.
It was also found that trans women had a 46 times higher risk of breast cancer than men in the general population. [xviii]
Third step: sex reassignment surgery from 18 years old
Male-to-female surgery includes the construction of external genitalia that look feminine (and removing the testicles). For the construction of a vagina, the scrotum is taken inside out. If puberty blockers have already been started at the very beginning of puberty, the scrotum is often too small and is supplemented with intestinal tissue. Often, the breasts are also enlarged. The Adam's apple can be made less prominent and the face can be feminised.
For female-to-male patients, the first surgery is often a mastectomy (this is allowed as early as at 16 years of age). The next phase is removal of the uterus and ovaries. A penis can be made by leading the urethra through the slightly enlarged clitoris or by forming a penis with a flap of skin from the forearm, for example. Not everyone chooses to undergo surgical construction of a penis, as the quality and functionality of a "neopenis" varies.
The operations which are currently possible do not confer the reproductive capacities or the same sexual function (e.g. the ability of having orgasms) of the opposite sex. This means that it is definitively no longer possible to have children naturally. Also, after the surgeries, lifelong hormone use is necessary. [xix]
Hazards
These operations are not without dangers. Urinary tract infections and problems with the urethra (fistulas and a narrowing of the opening) may develop.
Large increase
In order not to discourage, discriminate against or put off the adolescents in question, many parents, teachers and, above all, mental health counsellors rush to affirm the adolescents' desire to engage in a sex-change process. Publicly, this leads, among others, to adolescents appearing in ''coming out'' items on radio and TV, enthusiastically affirmed by loved ones and teachers. This enthusiasm and social encouragement could be contagious for other adolescents to explore the same path.
Three times as many girls
What is striking is the greater increase - since 2012 - in the number of girls knocking on the clinic's door. What could be the cause? Teenage girls go through a lot and often feel they don’t fit in. They struggle with anxiety, depression or eating disorders. They immerse themselves in social media, with unhealthily perfect pictures and discover transgender gurus. They share these experiences with friends and light each other up, research shows. This form of gender dysphoria is called 'Rapid Onset Gender Dysphoria', because it comes on suddenly. [xx]
Regret
This played out recently in a court case in the UK. Keira Bell was born a girl. Around the age of 14, she became confused about whether she was really a woman. Two years later, she started the transition process and around the age of 20, she had her breasts surgically removed. Later, she regretted it and took legal action against the gender clinic.
The question before the Supreme Court was whether a teenager like Keira has the faculties to consent to the use of puberty blockers. According to Keira, the gender clinic should have questioned her more deeply about her thoughts that she wanted to be a man.
The court agreed with Keira and ruled that it is "highly unlikely that a child of 13 years or younger would be able to consent to the administration of puberty blockers. It is doubtful that a child of 14 or 15 could understand and weigh the long-term risks and consequences of the administration of puberty blockers."
The issue is also that, when autism plays a role among these young people, there is an increasing number of voices indicating that these young people are experiencing delayed development compared to their peers, in several areas, including the development or interpretation of their sexuality, and may therefore potentially be even less able to make these lifelong decisions than their peers.
A day after the Supreme Court ruling, a long-term study was published by the English Gender Clinic. This showed that treatment with pubertal blockers did not improve psychological functioning. [xxi]
Turn back
The court ruling is bound to drastically reduce the number of gender treatments for adolescents in the UK. Such a turnaround can also be seen in Finland, France, Norway and Sweden. In Sweden, a survey of the general population showed that medical transition (gender reassignment), with or without surgery, did not reduce mood or anxiety disorders. On the contrary, treatment for anxiety disorders was more common among people who had undergone gender reassignment surgery. This resulted in more emphasis on the importance of psychological treatment and a decrease in the number of medical transitions.[xxii]
Psychological help
All of this is in line with what leading psychiatrists say: look at the - often common - underlying problems and treat the mental disorders or symptoms. Then, 80 - 90 per cent of the children will get over gender dysphoria. [xxiii] So far, to improve the long-term mental and physical health or social and romantic happiness of young people, no treatments have been found to be more effective than psychotherapeutic approaches.[xxiv]
Ethical considerations
The lack of conclusive medical evidence of the therapeutic effect of gender-affirming treatments, together with the large increase in the number of teenagers - especially girls - coming to gender clinics in recent years, makes the need for ethical reflection urgent.
Can someone's request for a treatment to adjust his/her body to the desired sex, with the sole intention of satisfying a desire, a treatment with unknown risks and side effects and (usually) irreversible consequences, be ethically acceptable?
Besides this core ethical question, treating teenagers raises a number of specific ethical questions too, such as: What is the right time to start transitioning? Who should make the decision? Can teenagers make this decision? And is this treatment proportionate?
The following section discusses the timing of treatment and the principles of autonomy and proportionality - ethical arguments relevant to the ethical assessment of the treatment of gender dysphoric children.
Timing
Decisive decisions with important implications for our lives must be made at the right time. Especially if these decisions not only affect our role in society but also change our identity, self-image and position in the world. Transitioning to the desired sex in people with gender dysphoria is undoubtedly one of these decisions. All the more so when it comes to treating teenagers, who are at the beginning of their lives.
Of course, one could name a number of advantages of starting the transition of teenagers struggling with transgender feelings as early as possible. First and foremost, it avoids the misery associated with going through puberty in the "wrong" sex. So, say proponents, the earlier you start, the more suffering you save. Yet gender dysphoria feelings disappear in most teenagers after puberty. This group would benefit more from restraint. Unfortunately, no diagnostic tools are yet available that indicate which children will grow over gender dysphoria and in which children it will persist. Diagnosis can only be established on the subjective experience of the child not feeling happy in his/her biological sex, which means that there is a large margin of error.
A misdiagnosis has major negative consequences for the child. An issue that of course, takes on a greater dimension in minors than in adults. Even if feelings are a good indication of dissatisfaction with one's own sex, they cannot provide clarity about the permanence of gender dysphoria. Diagnosis gender dysphoria in minors thus involves great complexity and difficulties [xxv].
The invasive nature of treatment makes it necessary to wait until a certain degree of certainty can be obtained. This is the purpose of administering puberty blockers, according to the Dutch protocol: this would buy time to further explore feelings and to be able to determine with clarity in which teenagers the feelings persist. However, as indicated above, the function of puberty blockers is not limited to delaying puberty but stands in the way of normal psychosocial and physical development of teenagers. As a result, the gender dysphoric feelings are confirmed; even in children who would normally grow over the gender dysphoria afterwards.
Autonomy
Due to the vulnerability of teenagers with gender dysphoria, the question of whether minors are able to consent to treatments with profound effects on their lives is a requirement in any clinical intervention. Being able to make informed autonomous decisions requires a certain maturity which teenagers in early adolescence do not have. At this young age, it is difficult to oversee the consequences of such a drastic treatment for the rest of their lives, especially since children with gender dysphoria often have psychological problems which interfere with the expression of their autonomy. Their immaturity and the difficulty of correctly assessing the consequences and alternatives of the proposed treatments is contrary to the respect for the principle of autonomy.
It should be added that the treatment is still in an experimental phase, as puberty blockers were developed for the treatment of children experiencing early puberty and are not intended for use in children without medical necessity (i.e. those not suffering from an organic pathology). Research with children is subject to strict regulations. In principle, the Medical Research Act (WMO) does not allow research with people under 16 years of age, unless the research can benefit the people involved. So far, there are no known physical disorders that can lead to transsexual feelings, this makes it difficult or actually impossible to objectively indicate the medical benefits of treatment. Even if the possibilities to conduct scientific research with minors have been widened since 1 March 2017, the uncertainty of the diagnosis, the still unknown long-term consequences and the irreversible nature of the treatment provide enough reason to consider the experimental treatment as non-proportionate.
Proportionality
Gender dysphoria is the only psychological diagnosis treated with both hormonal and surgical therapy. In principle, the discomfort experienced by children with gender dysphoria could be resolved by adapting their feelings to their bodies. Yet, usually the solution of adapting the body to the feelings is chosen. The moral justification for this choice is based on two assumptions: first, that there is no moral difference between allowing puberty to continue naturally or adapting it through medication; second, that it is possible to improve psychological well-being through medical intervention that is not aimed at curing or correcting a physical abnormality. None of these assumptions is morally neutral. Inhibiting the normal development of puberty with subsequent hormonal treatment and surgery causes irreversible damage to the body. This has serious consequences for the fertility and sex life of adolescents who are not yet able to grasp the significance of this damage, as well as a shorter life expectancy due to a higher risk of cardiovascular disease.
Healthcare providers have a duty and the responsibility to safeguard the best interests and welfare of minors by protecting them and avoiding unnecessary suffering. Their personal welfare is at stake. Facilitating access to medication or surgery is too one-sided a solution for very complex situations. Together, we need to consider which options are available to promote the integral development and well-being of young people.
[i] Diagnostic and Statistical Manual of Mental Disorders (DSM-5)
[ii] American Psychiatric association, Highlights of Changes from DSM-IV-TR to DSM-5
[iii] Drescher, New Diagnostic Codes Lessons Stigma for Transgender People, Medscape, 9/11/2017
[iv] Reed GM, Drescher J, Krueger RB, Atalla E, Cochran SD, First MB, Cohen- Kettenis PT, Arango-de Montis I, Parish SJ, Cottler S, Briken P, Saxena S. Disorders related to sexuality and gender identity in the ICD-11: revising the ICD-10 classification based on current scientific evidence, best clinical practices, and human rights considerations. World Psychiatry. 2016 Oct;15(3):205-221. doi : 10.1002/wps.20354. Erratum in: World Psychiatry. 2017 Jun;16(2):220. PMID: 27717275; PMCID: PMC5032510.
[v]Arnoldussen, M., Steensma, TD, Popma, A. et al. Re-evaluation of the Dutch approach: are recently referred transgender youth different compared to earlier referrals? Eur Child Adolesc Psychiatry 29, 803–811 (2020)
[vi] MJ Heineman et al. (eds.), Obstetrics and gynecology . The Reproduction of Man; with a led by PE Treffers
[vii] Sarah‐Jayne Blakemore, Stephanie Burnett, Ronald E. Dahl, The role of puberty in the developing adolescent brain. 14 May 2010. Human Brain Mapping 31:926–933 (2010)
[viii] Life Sciences and Society Cahier 1 | 2019 | 38th volume Brain in growth
[ix]T. Vrouenraets et al., Trajectories of Adolescents Treated with Gonadotropin Releasing Hormone Analogues for Gender Dysphoria Archives of Sexual Behavior (2020) 49:2611–2618
[x] www.scientias.nl/transgenders-van-geslacht-veranderen
[xi]ALC de Vries, ThD Steensma, ThAH Doreleijers , PT Cohen- Kettenis , Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med, 2011 Aug;8(8):2276-83.)
[xii] https://www.transvisie.nl/transitie/jongeren/kinderwens/#1596366566813-4b76e92f-5ad4
[xiii]MC Vlot et al, Effect of pubertal suppression and cross-sex hormone therapy on bone turnover markers and bone mineral apparent density (BMAD) in transgender adolescents, in ScienceDirect, Vol. 95, February 2017, p. 11-19
[xiv]Michael K. Laidlaw, The Pediatric Endocrine Society's Statement on Puberty Blockers Isn't Just Deceptive. It's Dangerous, in Public Discourse, The Journal of the Witherspoon Institute, January 13, 2020 https://www.thepublicdiscourse.com/2020/01/59422/
[xv]ALC de Vries et al., Challenges in Timing Puberty Suppression for Gender-Nonconforming Adolescents. Pediatrics Oct 2020, 146
[xvi]http://psychopharmacologyuvt.pbworks.com/w/page/117419991/Genderdysphoria%20en%20depression
[xvii] NiM . Nota et al. , Occurrence of Acute Cardiovascular Events in Transgender Individuals Receiving Hormone Therapy. Circulation 2019;139:1461–1462
[xviii]CJM de Blok et al., Breast cancer risk in transgender people receiving hormone treatment: nationwide cohort study in the Netherlands BMJ 2019; 365:1652
[xix]https://www.vumc.nl/zorg/expertisecentra-en-specialismen/kennis-en-zorgcentrum-genderdysforie/informatie-voor-patienten-kennis-en-zorgcentrum-genderdysforie/phase-3-operating.htm
[xx]Littman, L., Parent reports of adolescents and young adults perceived to show signs of a rapid onset of gender dysphoria, PLOS One 2018.
[xxi] Polly Carmichael, Gary Butler, Una Masic , Tim J Cole, Bianca L De Stavola , Sarah Davidson, Elin M. Skageberg , Sophie Khadr, Russell Viner. Short-term outcomes of pubertal suppression in a selected cohort of 12 to 15 year old young people with persistent gender dysphoria in the UK
[xxii]Richard Bränström , Ph.D., John E. Pachankis , Ph.D., Reduction in Mental Health Treatment Utilization Among Transgender Individuals After Gender-Affirming Surgeries: A Total Population Study, the American Journal of Psychiatry, 04OCT19
[xxiii]MK Laidlaw et al., Letter to the Editor: “Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline”, The Journal of Clinical Endocrinology & Metabolism, Volume 104, Issue 3, March 2019, Pages 686–687
[xxiv] Dr. Stephen B. Levine, MD, Expert Affidavit Case 2020CV000454, Doe v. Madison Metropolitan School District, Circuit Court, Dane County, WI, p.35